ACNE TREATMENT
What Causes Acne?
There isn't a simple answer to this question. To make sense of the causes of acne it helps to break down the discussion into general topic areas.
Genetics Play a Central Role in the Development of Acne
Genetic makeup is the dominant factor determining an individual's likelihood of developing acne. Genetics impact structure of the hair follicle, sebaceous gland activity, hormone levels and the immune response to bacteria. For example, many people who suffer from inflammatory acne have immune cells that are less effective at killing the acne bacteria or produce more inflammatory molecules than the general population – as a result, their body responds more vigorously, but less effectively, to acne causing bacteria, resulting in increased inflammation.
Propionibacterium acnes are the bacteria most often associated with Acne Vulgaris. Acne, particularly inflammatory acne is usually the result of bacterial growth deep within the hair follicle. These bacteria produce molecules which incite an immune response, leading to inflammation and acne symptoms. The more bacterial growth there is, the more likely an individual will develop acne symptoms. The bacteria primarily responsible for acne is Propionibacterium acnes (P. acnes), but other bacteria such as Staphylococcus aureus can also live on the skin and in hair follicles. There are many different strains of P. acnes bacteria, however, and many of these strains have developed resistance to one or many different antibiotics. As a result, some antibiotics, including erythromycin and tetracycline, are becoming less effective, because many people who suffer from acne carry strains of bacteria that are resistant.
Acne at the Cellular Level
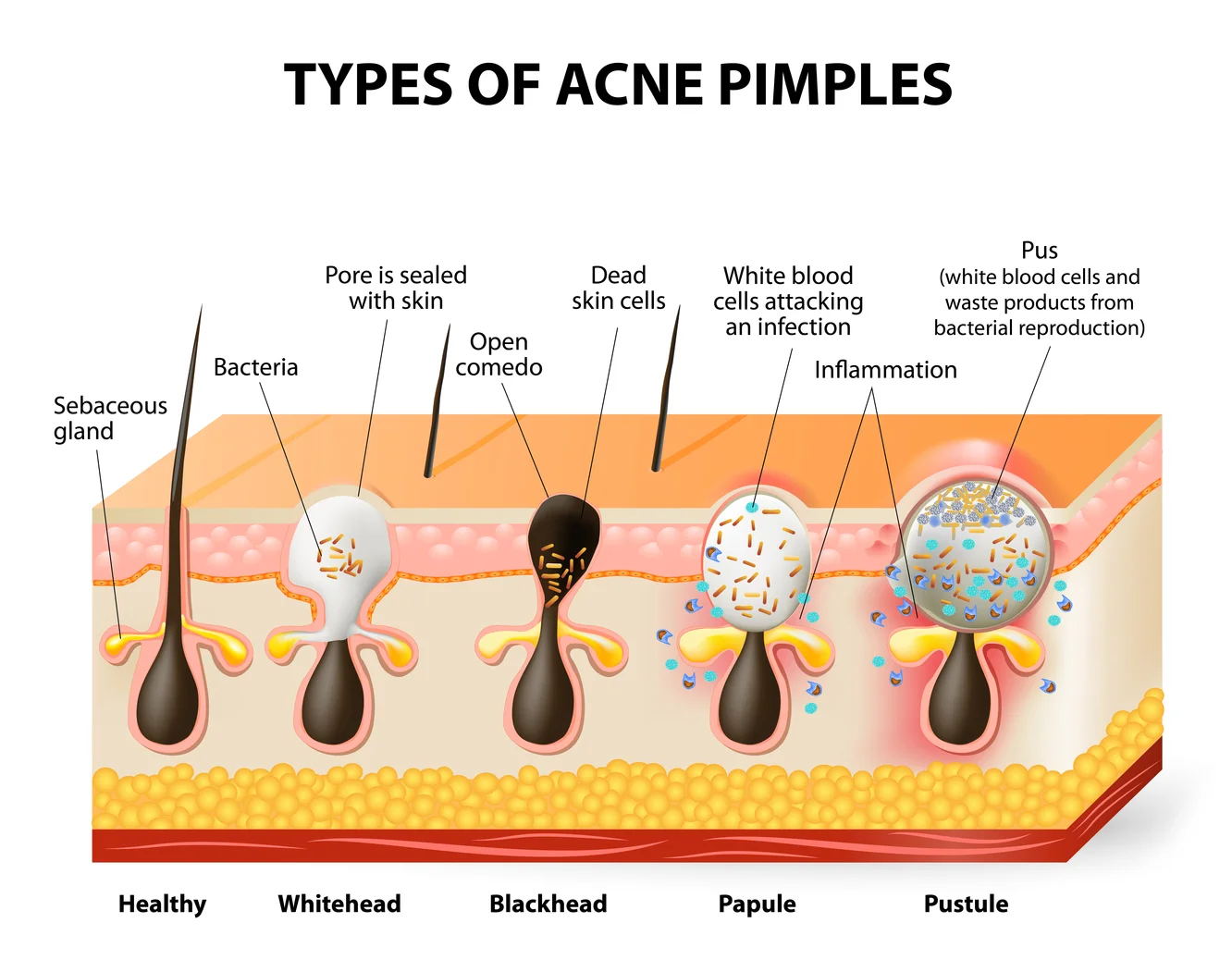
At a very basic level, acne results from a combination of factors that result in blocked pores, an accumulation of sebum, bacterial growth and inflammation. Acne generally occurs within the hair follicle, when excess sebum is produced by the sebaceous glands and creates a plug that blocks the follicle. This plug creates a micro-environment that favors the growth of certain types of bacteria, such as Propionibacterium acnes and Staphylococcus aureus. The presence of these bacteria triggers an immune response, which is characterized by inflammation, increased blood flow (redness) and the recruitment of white blood cells to the follicle. Primary inflammation can often cause additional damage to the follicle and surrounding tissue, allowing proliferation of the bacterial infection and in turn inducing further swelling. In some individuals, this process becomes a vicious cycle and leads to extensive acne and significant damage to the skin and the subcutaneous tissue.
The Sebaceous Glands
In a healthy follicle, the sebaceous gland produces the appropriate amount of sebum to maintain the health of the hair and surrounding tissue, and that sebum is efficiently extruded along with the hair. In people that suffer from acne, several things can happen that disrupt this delicate balance. Normally, the sebaceous glands are relatively small and produce a minimal amount of sebum. However, in many cases of acne, the primary culprit is an overproduction of sebum. In some cases, the sebaceous glands grow larger and produce greater amounts of sebum. Excessive growth and proliferation of the sebaceous glands is known as sebaceous hyperplasia. Sebaceous hyperplasia is triggered by increases in androgen hormones, as happens during puberty.
Sebum
Sebum itself is created by the breakdown of the cells that form the sebaceous gland. Sebaceous cells replicate at the base of the gland and move up towards the hair follicle as the new cells proliferate. As the maturing cells approach the hair follicle, they undergo apoptosis and die. The cells are lipid rich (oil) and the byproducts left over as the cells dissolve composes the sebum that lubricates and protects the hair. Proliferation of the sebaceous glands causes an increase in the production of sebum, which is often manifested as oily skin and hair. The sebum can also serve as a nutrition source for bacteria that are capable of living in the hair follicle, such as P. acnes and S. aureus. Excess amounts of sebum can encourage bacterial growth and lead to inflammation, redness and an infiltration of white blood cells (pus). If the plug in the hair shaft is located near the surface, this process can often lead to the formulation of a surface pustule (whitehead). However, for many people who suffer with nodular and cystic acne, the pustules are often formed deep in the tissue and away from the surface.
Inflammation
The formation of a plug in the follicle can lead to the accumulation of sebum, bacteria and white blood cells deep within the follicle. In these cases, the result is often the formation of large painful nodules and cysts. Since the pustule is surrounded by tissue, it is not easily able to drain the pus and bacteria to the surface. Many times, continued sebum production, bacterial growth and inflammation within a plugged follicle can cause the follicle to rupture and drain into the surrounding tissue beneath the skin's surface. This process can lead to further inflammation, dissemination of the bacterial infection and progression of the disease. This cycle of infection, inflammation and damage is also responsible for the formation of acne sca
Types of Acne
Type 1 Acne Minimal inflammation, minimal affected area, not painful, irregular outbreaks.
Type 1 acne is the most mild form of acne and generally is the least damaging and easiest to treat form of the disease. It is characterized by a lack of inflammation and is usually not particularly painful. The area of the body affected by the acne is usually limited. This type of acne is often transient and often resolves on its own after about a week. Non-inflamed blackheads and small red bumps (papules) are common with this form of acne which appears to be particularly common in females and often affects the forehead, cheeks, nose and neck.
Type 2 Acne Mild inflammation, some painful pimples, regular outbreaks.
A common manifestation of the disease, Type 2 acne is similar to Type 1 acne, but is characterized by increased levels of inflammation and redness. Pimples can range from small red bumps to medium sized whiteheads. Unlike Type 1 Acne blemishes, the increased inflammation causes pimples that are often painful to the touch. Over the counter topical treatments are often partially effective at decreasing the severity and duration of outbreaks, but are frequently inadequate. It is important to practice good hygiene and avoid exacerbating the situation by "popping" pimples.
Type 3 Acne Large, painful pimples, nodular pimples, frequent outbreaks.
Type 3 Acne is characterized by the presence of midsized to large nodules and pustules that are frequently painful. In Type 3 Acne, pimples are often associated with significant inflammation. Large whiteheads and large, painful red bumps are common. Individual pimples can often take longer to resolve, up to 10 - 14 days. In type 3 Acne, much of the inflammation and infection originates deeper in the tissue than in Types 1 and 2, often localizing in the dermis and sub-cutaneous fatty tissue. Because of this, type 3 Acne is usually unresponsive to over the counter topical medications. Likewise, the efficacy of topical antibiotics and topical retinoids is often limited. In many cases, oral antibiotics and oral retinoids are often prescribed as treatments for Type 3 acne. The increased inflammation associated with Type 3 acne poses a significant risk of permanent scarring. Deep seated nodules and pustules can cause damage to the structural matrix that underlies the skin, causing pitting, discoloration and the accumulation of scar tissue.
Type 4 Acne Large & painful nodules, pustules and cysts, persistent outbreak.
The most severe form of the disease, Type 4 Acne almost invariably causes permanent skin damage and scarring. Like Type 3 Acne, Type 4 Acne is characterized by a deep seated infection and extensive inflammation. Large cysts, which are essentially large, irregular nodules are a common feature in Type 4 Acne. Type 4 acne is usually completely non-responsive to over the counter medications. Topical antibiotics and retinoids are minimally effective, in most cases. Type 4 Acne can cause extensive damage to the skin and underlying structure, causing heavy scarring if left untreated. Type 4 acne is often extremely painful, both physically and emotionally, and should be treated as early and aggressively as possible.
Type 1 Type 2 Type 3 Type 4